What We Learned When My Fiancé Was Hospitalized For Life-Threatening Anemia
What is anaemia, what causes it, and how can we prevent it?
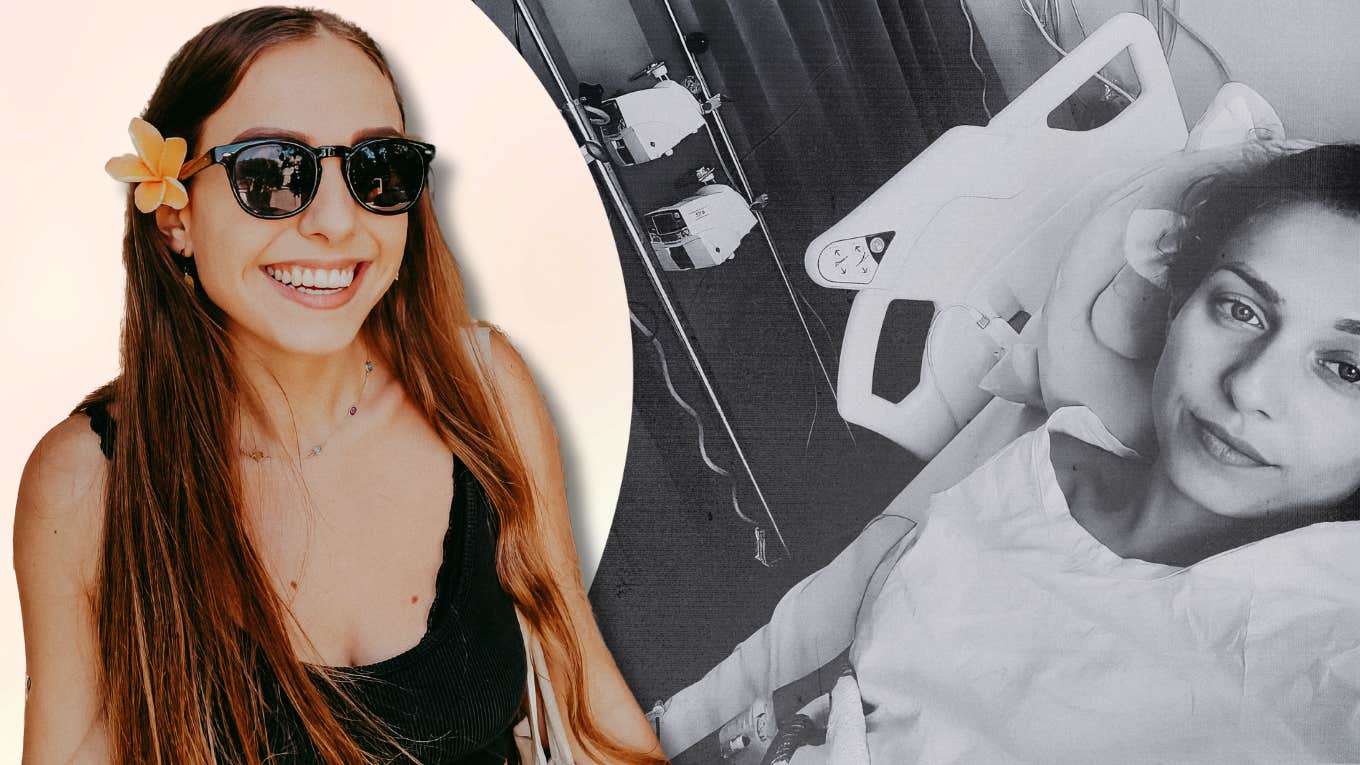 Courtesy Of Author
Courtesy Of Author My fiancée Ilayda was at work when our doctor called. “Stay calm and don’t rush,” Dr. Su said, “but you need to go straight to the hospital because you’re severely anemic and in danger of heart failure.”
After a few weeks of feeling fatigued, out of breath, unusually cold, occasionally dizzy, and having an elevated heart rate, we already knew something was wrong, but we weren’t prepared for such shocking news.
 Photo by author
Photo by author
Ilayda had dangerously low levels of hemoglobin and red blood cells and needed emergency blood transfusions.
For a young, healthy 26-year-old woman, the normal range of hemoglobin is around 119–160. Ilayda’s hemoglobin count was 54. Her red blood cells told the same story. The healthy range is 3.8–5.8, and her red blood cell count was 2.5.
 Photo by author
Photo by author
Our local doctor and the staff at the hospital were shocked by the numbers, the lowest they’d ever seen. It was scary to hear and see their astonished reactions — not a Christmas surprise anyone had hoped for.
Fortunately, Australia has one of the best publicly-funded healthcare systems in the world. Within an hour, we were at the hospital surrounded by nurses, doctors, and machines making unsettling beeping sounds.
Ilayda stayed in the hospital for four days and received world-class care, and it was all covered by Australia’s public healthcare scheme, Medicare. By comparison, healthcare costs in the United States are the leading cause of bankruptcy.
Frightening as it was, Ilayda now feels better; her vital signs are all in a healthy range, and we’re lucky to have a wonderful local doctor looking after her — thanks, Dr. Su!
 Photo by author
Photo by author
But how could this happen to an otherwise healthy young woman in the prime of her life? And how can we make sure she stays healthy?
We learned a lot about these questions and want to share what we found so that others can avoid these dangers as well.
Here are 4 lessons we learned when my fiancée was hospitalized for life-threatening anemia:
1. What is anemia?
Anemia occurs when our hemoglobin and/or red blood cell count drops below the healthy range.
Haemoglobin is an essential protein found in red blood cells. Because it contains atoms of iron, which are positively charged, hemoglobin attracts and binds oxygen, which is negatively charged.
This is how our circulatory system ferries oxygen around our bodies to feed metabolism in our trillions of cells. Around 35 trillion red blood cells travel around our body to deliver their cargo of oxygen. They then travel in a full circuit back to our lungs, where they’re resupplied with oxygen and continue the cycle.
As a helpful metaphor, imagine our blood vessels as a railway system, where trains are red blood cells and passengers are oxygen.
2. What causes anemia?
Sadly, there are many roads to anemia, and it’s one of the most common conditions worldwide.
For example, anemia can be caused by an array of conditions in which our bodies don’t produce enough red blood cells and/or hemoglobin. This can be because they are produced too slowly, they don’t survive as long as they should, or they’re defective in some way (e.g., sickle cell anemia).
Anemia can also be caused by loss of blood, like during heavy menstrual periods. This is one of the reasons why anemia is more common among women than men.
Another path to anemia involves deficiencies in various essential vitamins, nutrients, and minerals, such as vitamin B12, folate, and iron.
For Ilayda, the culprit was fairly obvious, as she was severely iron deficient. By contrast, her levels of vitamin B12 and folate were very healthy. The normal range of iron (5–30) is quite wide to begin with, and yet her iron levels were only 1.3, well below the minimum.
Since iron is an essential component of hemoglobin, iron deficiency means we can’t produce enough hemoglobin to carry oxygen around the body. Iron deficiency is the most common cause of anemia.
3. How can you treat anemia?
During her four days and nights in the hospital, Ilayda received three blood transfusions (750mL total), an infusion of iron (1L total), and three infusions of nutrient-rich water (3L total).
 Photo by author
Photo by author
Within 24 hours of arriving at the emergency department, her red blood cell and hemoglobin counts were quickly rising to healthy levels. After three days, all of her vital signs were in a healthy range, and she was released with a clean bill of health the following afternoon.
Our local doctor, Dr. Su, explained that red blood cells live for about 120 days. That means the blood Ilayda received will gradually fade from her system and will need to be replaced by her body (most red blood cells are made by our bone marrow).
Dr. Su scheduled a blood test for a month from now. If Ilayda’s red blood cell and hemoglobin counts are normal, that will indicate her body is producing enough on its own.
 Photo by author
Photo by author
If not, we’ll need to take another spin around the merry-go-round of medical tests until we find the problem. But so far Ilayda feels great, so let’s hope it doesn’t come to that.
4. How can you prevent anemia?
As you’d expect, the doctors said to eat more foods rich in iron. But dietary iron comes in different forms, depending on whether you’re eating plants or meat/eggs.
The iron found in meat and eggs (‘haem iron’) is more efficiently absorbed than the iron contained in plants (‘non-haem iron’). The ‘bioavailability’ of animal-based iron is roughly 25–30%, while plant-based iron is only 1–10%.
Ilayda tends not to eat a lot of meat — although, as a devout German, she does love döner kebabs. However, given the importance of meat-based iron, she’s learning to become more of a carnivore.
But overconsumption of red meat can increase our risk of heart disease and bowel cancer, so it’s important to eat plenty of iron-rich plants as well, like leafy greens, legumes, and iron-fortified cereals. If possible, it’s best to combine the two, as animal-based iron helps our bodies to absorb plant-based iron. Vitamin C is another useful tool, as it also helps our bodies absorb iron.
If dietary strategies aren’t enough, iron supplements are another option. But iron supplements usually don’t cover our needs, so they aren’t a substitute for iron-rich food.
 Photo: bit245 | Canva
Photo: bit245 | Canva
It’s a massive relief that successful dietary and supplemental strategies are available. However, we should mention that this is problematic in poorer parts of the world, where sources of dietary and supplemental iron are far less abundant and less affordable than in much of the West. I witnessed this myself when I volunteered with a human rights NGO in Thailand. We ran a center for poor and stateless children, and I saw first-hand how disadvantage can lead to malnutrition and disease.
Given her many symptoms over the preceding weeks, we already knew something was up, but we never expected that her life might be in danger. It was a very cold splash of water on our unsuspecting faces, and in our darker moments, we worried about what might happen.
 Photo by author
Photo by author
But we’re lucky to live in a country with an affordable and high-quality medical system. Ilayda feels better than ever. We’ve got the support of good doctors, and we have a simple plan to keep her healthy.
If you or someone you care about feels unwell like Ilayda did, make sure to go to a doctor for a check-up.
 Photo: Mayoclinic
Photo: Mayoclinic
If you are one of the billions of people who struggle with anemia, eat plenty of iron-rich foods. Animal-based iron is most easily absorbed, but we also need to eat lots of iron-rich plants. Vitamin C helps us absorb iron, and if iron from food isn’t enough, we can take iron supplements. If you need help designing the right diet or finding an iron supplement, speak to your doctor and/or nutritionist.
Last but not least, from the bottom of our hearts, thank you to all the blood donors out there. Where would we be with you?
Dr. Matt Williams-Spooner is an evolutionary neurobiologist who studies the neuroscience of behavior. He also writes articles about science and health on Medium.

